My Smear Test Came Back Abnormal, Now What?
An abnormal smear result usually means that minor changes were found in the cells in the surface membrane of the cervix. It takes many years for these abnormalities to develop into cancer but with regular screenings, cell changes that could cause cancer in the future can be picked up at an early stage.

Booking in for your smear test can be a journey. The thought of having to put your vagina in the face of a stranger, albeit a gloved-up professional one, does not usually make for a relaxing situation alas, it’s the best way to check the health of the cervix and to detect high-risk Human Papillomavirus (HPV) or precancerous abnormalities.
If your cervical screening shows abnormal results, don’t panic (easier said than done, we know). Whilst 1 in 20 people with cervix will have an abnormal smear test result only 1 in 2000 will have cervical cancer.
An abnormal smear result usually means that minor changes were found in the cells in the surface membrane of the cervix, known as squamous cells. It takes many years for these abnormalities to develop into cancer but with regular screenings, cell changes that could potentially cause cancer in the future if left untreated can be picked up at an early stage. That’s why attending your smear test is so important!
To sort the facts from the fiction and make your next routine smear more bearable, we spoke to Senior Consultant Obstetrician and Gynaecologist, Dr Nitu Bajekal to find out what to expect when you get an abnormal test result.
The importance of attending cervical screening
Understanding why we’re invited for a smear test in the first place and what they’re looking for when they’re shining a bright light up there can be, well, enlightening!
Whilst it’s hardly going to feature on your ‘three positive things that happened today’ list, knowing exactly why you’re going can help take the stress out of the appointment and put your mind at ease.
There are plenty of reasons why someone wouldn’t want to attend a screening, whether it be down to embarrassment, concerns about the results or if the procedure will be painful and even access to convenient screening times, but showing up for yours is your best chance of preventing cancer.
Cervical screening tests for a virus called human papillomavirus (HPV) and virtually all cases of cervical cancer are linked to high risk HPV.
Cervical cancer is the second most common cause of cancer in women. It is also the most common cancer in women under the age of 35.Dr Nitu Bajekal
Dr Nitu Bajekal explains: “Cervical cancer is the second most common cause of cancer in women. It is also the most common cancer in women under the age of 35. Types 16 and 18 are strains of high-risk HPV responsible for 70% of all cervical cancers while low risk HPV strains can cause genital warts. “Apart from cervical cancer, high risk HPV can also cause vaginal and vulval cancers in women as well as head and neck cancers, penile and anal cancers, especially in men who smoke and drink alcohol in excess. Women and men who are sexually active do need to be aware of the correlation between HPV infection and cancer as there is help available. The good news is that cervical cancer is almost completely preventable.”
If every eligible woman or person with a cervix attended cervical screening, 83% of cervical cancer deaths could be prevented (Cancer Research UK).

Pap test, smear test and cervical screening – what does it all mean?
The terminology used to refer to the test itself can be reason enough to feel confused and worried about attending yours. Essentially, they’re all synonyms for the same thing as Dr Nitu Bajekal explains, “A smear test is also known as cervical screening, cervical smear or Pap or Papanicolaou Smear or Pap test (after Dr Georgios Papanikolaou, a Greek physician, one of the pioneers in the early detection of cervical cancer).
Cervical cancer is caused by a virus (HPV) and is 99.8% preventable if detected before the cells changeDr Nitu Bajekal
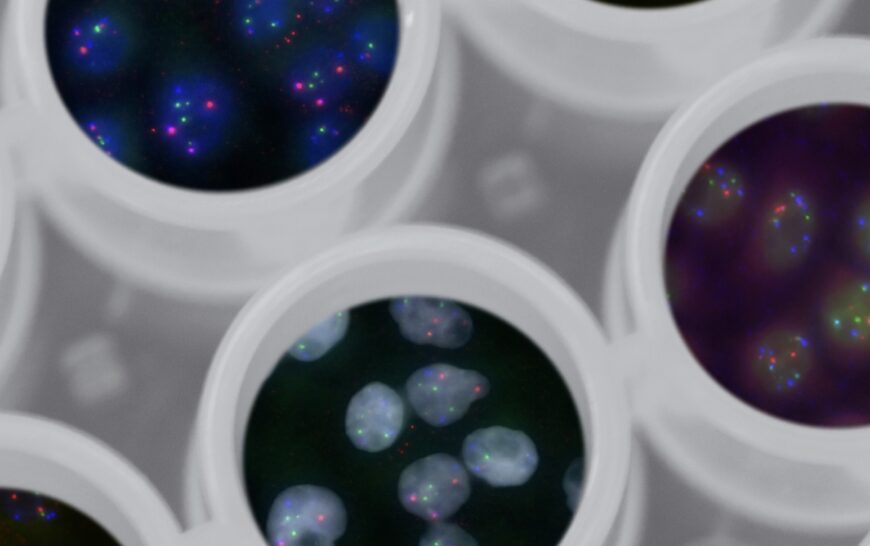
“The smear test is still used as one of the main forms of cervical cancer screening in most parts of the world and involves collecting cells from the cervix and examining them under a microscope to detect abnormal cells long before they turn cancerous. This is important as cervical cancer is caused by a virus (HPV) and is 99.8% preventable if detected before the cells change and highly treatable the earlier changes in the cervix are detected. These terms are all synonyms and used interchangeably, with some names more popular in some countries.”
A smear test is NOT to detect cancer
It’s a common misconception that the purpose of having a smear test is to detect cancer but cervical screening is used to detect abnormal cells years before they turn cancerous. It is a test to help prevent cancer.
“A smear test is not used for detection of cervical cancer but is a screening tool to highlight those people with a cervix that need to be referred for further tests if abnormal cells are detected on a smear,” says Dr Nitu Bajekal.
Let’s talk abnormalities
Getting an abnormal result can be daunting – it’s natural to be concerned about the severity of your cell changes and the implications this may have on your health – but it does not mean you have cancer. The result represents a precancerous abnormality on the cervix.
“For every 100 women or those assigned female at birth (AFAB) people who have a smear test, 94 will have a normal result (negative or clear smear) and return to routine recall. Six of them will have an abnormal test. Two will have no evidence of HPV infection and will return to the NHS national protocol of smear tests every 3 years from age 25-49 and every 5 years from age 50-64 if smears have always remained clear or negative for changes. Four people with a cervix will have precancerous cells of various grades (low or high-grade dyskaryosis) and will need to be referred for a colposcopy (a colposcopy involves inspecting the cervix with a special type of magnifying instrument),” says Dr Nitu Bajekal.
Possible reasons for an abnormal smear result
“The most common reason for an abnormal smear test is the detection of early precancerous cells, known as low-grade dyskaryosis. A small group will have higher grade changes (high-grade dyskaryosis or detection of high-grade glandular changes),” says Dr Nitu Bajekal.
Other factors can also affect a smear result from pregnancy to menopause and blood. “Sometimes excess vaginal discharge, vaginal infections or blood contaminating the smear test may initially suggest an abnormal result such as a borderline or inadequate result (smears are ideally performed mid-cycle when plenty of cells are obtained and not during a period). Menopause, when periods have stopped cause a drop in oestrogen levels which can make the vaginal/cervix tissues atrophic (thinned out) so enough cells are not obtained in the sample from the neck of the womb and the result is known as inadequate. Pregnancy / postpartum (6-8 weeks) can also result in not having a clear smear report. However, in almost all these situations, the HPV test is negative, which means the person can be reassured.”
If there are symptoms of bleeding after vaginal sex, bleeding in between periods or pelvic pain, Dr Nitu Bajekal suggests seeking urgent medical advice, even if it is just for reassurance. Don’t wait for your routine smear.

Understanding high-risk HPV
Human Papillomavirus is the most common sexually transmitted infection and is usually harmless, but some types can lead to skin warts, genital warts and some forms of cancer, including cervical cancer.
It has been estimated that 75%-80% of sexually active adults will acquire at least one genital HPV infection before the age of 50Dr Nitu Bajekal
“HPV infection is caused by a group of over 100 different types of HPV; more than 40 of these are known to infect the cervix, and approximately 15 are known to cause cervical cancer. The HPV types are classified as being high or low risk for causing cervical cancer. HPV infection is the underlying cause of abnormal cervical smears. Certain strains of HPV known as High-Risk HPV are responsible for almost all cases of cervical cancer. Almost everyone who is or has been sexually active will get infected with the HPV virus at some point in their lifetime. It has been estimated that 75%-80% of sexually active adults will acquire at least one genital HPV infection before the age of 50. It is more common in young people, but no age is exempt. By building natural immunity, in time most people will clear the virus from their system within two years.
“Most people have no symptoms from the HPV infection and clear it on their own.”
However, for some people, the virus remains dormant in the body and if it is High-Risk HPV, it can cause changes in the neck of the womb known as dyskaryosis (low/high-grade changes) and precancerous cells may develop (Cervical Intraepithelial Neoplasia CIN 1,2,3) which over several years may turn into cervical cancer in a small minority over several years. It is usually not possible to trace the source of the HPV infection, as it may have been lying silent for several years before any symptoms are experienced.”
CIN grading
CIN refers to Cervical Intraepithelial Neoplasia, these are pre-cancerous changes within the lining cells of the neck of the womb.
There are three grades of CIN (CIN1, 2 & 3). CIN1 is considered low grade and CIN2 and CIN3 are high grade changes and need to be treated to prevent future risk of cervical cancer whereas minor changes such as CIN1 will often resolve on its own and revert to normal as the HPV clears.
I have an abnormal result, what happens next?
Scenario one
- Primary HPV testing from age 25 in the UK
- Tested for the presence of certain strains of HPV known as HRHPV (High- Risk HPV)If negative for HRHPV, no further tests required.
- Back to Routine 3-5 yearly recall.
Scenario two
- Primary HPV testing from age 25 in the UK
- Tested for the presence of certain strains of HPV
- If positive for HRHPV, then the cells are examined for changes (dyskaryosis). These can then be treated before they get a chance to turn into cervical cancer.
- If it is clear or negative for cell changes, a smear and HPV test is recommended in 12 months in most situations.
Scenario three
- Primary HPV testing from age 25 in the UK
- Tested for the presence of certain strains of HPV
- If positive for HRHPV and cells examined show evidence of changes (low grade or high grade dyskaryosis), referred to colposcopy where the cervix is assessed under magnification for precancerous cells (Cervical Intraepithelial Neoplasia CIN 1,2,3 – CIN 1 considered low grade and CIN 2and CIN 3 as high grade).
More on colposcopy
“Colposcopy is part of a screening programme to ensure the cervix stays healthy. Your smear test has shown some changes in the cells, or you have tested positive for some of the HPV strains. In many cases these changes return to normal without treatment but sometimes the changes become worse and could lead to cancer in the future. We sometimes call these cells, precancer or early warning cells. As there is no way at present of knowing whose cells will get better or worse, it is wise to monitor everyone who has these changed cells, as a preventative measure.
“If there is no biopsy indicated and the cervix shows just minor changes, you may be asked to return in a year’s time for a further smear test as many women will clear the virus spontaneously. Depending on the results of the cervical biopsy, you may be advised just monitoring or to have treatment (LLETZ – Large Loop Excision of Transformation Zone) to remove the abnormal cells under local or a short general anaesthetic.”
What happens in the event of high-grade changes?
“If this is the case, a treatment to remove the abnormal cells with high-grade changes from the cervix is recommended (LLETZ, LEEP, Loop diathermy). This is usually an office or outpatient procedure performed under local anaesthetic, or local anaesthetic and sedation or under a short general anaesthetic as a day case depending on the patient’s wishes and certain findings at colposcopy (such as previous treatment, large lesion, highly anxious patient, difficult access).
“A deeper treatment such as a cone biopsy may be recommended, or occasionally if LLETZ or cone biopsy is not appropriate or the person has additional genealogical problems, a hysterectomy may be advised after all other options have been considered. These decisions are not taken lightly and only after a review of the entire medical history, the biopsy findings, and the patient’s wishes in a multidisciplinary team meeting (MDT). Similarly, in any case, that has unusual findings or if the patient is very young, discussions by a team of experts ensure the best treatment outcome for the patient.”
Treatment methods
“Ablative treatment such as freezing or cryotherapy is generally not a preferred option in the UK as there is no tissue removed to analyse that all precancerous abnormal cells have been removed, unlike the above procedures which are excision procedures where tissue that is removed is sent for detailed analysis by the histopathologist.”

Loop electrosurgical excision (LEEP) or LLETZ as known in the UK
“An LLETZ (Large Loop Excision of the Transformation Zone), also known as LEEP (Loop Electrical Excision Procedure) or a loop diathermy procedure, is most commonly performed under a local anaesthetic to remove abnormal cells from the cervix. A cold knife cone biopsy is sometimes performed instead of an LLETZ procedure to remove abnormal cells, depending on the nature or type of cells seen. Your doctor will guide you as to the best option for your situation. The procedure takes a few minutes, with the entire appointment taking between 20-30 minutes, to ensure you are comfortable and the local anaesthetic is working properly.
“After treatment, in most situations, once the cells removed have been analysed to confirm there are no serious concerns, you will be invited for a TOC test (test of cure) in six months. This is a smear test to confirm you have gotten rid of the HPV infection and that there are no persisting abnormal cells. You will be advised of the results of the tissue removed at the LLETZ procedure. Depending on these results, further management will be decided. You will usually be followed up with a smear in 6 months (Test of Cure). Most women will return to normal recall for smear tests. Further, follow up with colposcopy or further treatment may be needed in some situations.”
What are the possible risks of treatment?
LLETZ is the most common treatment for cervical cell changes. It uses a thin wire loop with an electrical current to remove the affected area of the cervix. Although it sounds petrifying, it’s a relatively straightforward treatment and you can always ask your colposcopist or GP before treatment if you’re concerned or want them to talk you through what to expect in your appointment.
As with any procedure, LLETZ has small risks but in many cases, the benefits outweigh the risks as Dr Nitu Bajekal explains:
“The procedure is only offered if it is thought to be in your best interests. The small risks include a 1 in 100 risk of heavy bleeding, or infection and a 5 in 100 risk of needing further treatment because of persistent abnormal cells or new abnormal cells developing in the future.
Most women feel fine after having treatment to the cervix, but a few may feel the need to go home and rest. Either way, it is recommended you don’t plan to do anything else that day.
You may have some period type pains for the rest of the day once the anaesthetic has worn off, and it seems that having pain seems to be more likely in women who haven’t had children. You may take your normal painkillers or paracetamol.
Bleeding
“You should expect to have some bleeding or discharge after this procedure, sometimes up to 3-4 weeks, with the amount varying depending partly on the type of treatment you have had. Some women have none. The bleeding may stop after a few days but start again 10-14 days later. This is the scab coming away and nothing to worry about. It will stop eventually. You may also notice that your next period may be slightly heavier than normal, and again, this is nothing to worry about. If you are on the contraceptive pill, I recommend that you take the pill back-to-back for a couple of months to avoid the heavier period if you so wish. This is safe to do.
“If you start to bleed very heavily, you should seek urgent medical advice. Infection can occur occasionally, but to minimise this, do not use tampons or have sex for three weeks after the procedure. Heavy exercise and swimming are also not recommended for three weeks. If you develop an infection (pain, high temperature, unpleasant smell and/or generally feeling unwell) you will need to seek medical advice urgently.
“Avoid vaginal intercourse for 3-4 weeks to avoid disturbing the healing wound and reduce risk of infection. You should be able to drive when you feel comfortable. You should wait for at least 24 hours after a general anaesthetic.”
Can treatment affect future pregnancies and fertility?
“There is no real risk to fertility. There is a very small increased risk of preterm labour (babies born before 37 weeks gestation) or needing a stitch in the cervix (cervical cerclage) as a result of weakness of the neck of the womb after treatment to the cervix. There is also a small chance that the cervix may not dilate as it should during labour (cervical dystocia) and a caesarean section may be indicated in such situations. These risks are slightly more common with cold knife cone biopsy.
“Depending on the results of the cells removed from the cervix and the amount of tissue removed from the cervix, you may be advised to inform your obstetrician so that you can be monitored during pregnancy and the length of your cervix measured by regular ultrasound scans to watch for any potential weakness developing. Recently, there has been some concern about sexual orgasm being affected after treatment. This is very uncommon and as mentioned, treatment is only offered when the benefits outweigh the risks. In my 35 years of practice as a gynaecologist, this has not been an issue for my patients who I have been following up for a while. However, I must stress all these risks are very small and should not deter from having necessary treatment.”
One thing Dr Nitu Bajekal would like everyone to know about smear tests!
1 in 3 women between 25-29 years don’t attend their smear tests. Dr Nitu Bajekal
“It can save your life. The NHS offers smears between the ages of 25-64 years unless there is a medical reason to do them more frequently. Sadly, 1 in 3 women between 25-29 years don’t attend their smear tests. Self-testing is accurate and is an area that is being developed to try and target those women who don’t come forward for routine cervical smear testing because they find these tests intrusive or don’t have the time to go to their doctor.” “There is a relationship between smoking and abnormal cells on the cervix. So, if you are a smoker, please consider giving up or cutting down. There is some evidence to suggest that even partners smoking may have an effect.”
Useful Resources
NHS, BSCCP, RCOG, www.nitubajekal.com , Jo’s cervical cancer trust.
You can also buy Dr Nitu Bajekal’s book here.
For more information on what to expect from a cervical smear test, check out our article on Dismantling The Fear of the Smear.





