“It feels like your mind is betraying you” – The Reality of Living With Obsessive Compulsive Disorder (OCD)
Living with OCD goes far beyond perfectionism, cleanliness and next-level organisation skills, and to suggest ‘being a bit OCD’ is a personality quirk is undermining the severity of the disorder.
Here in the UK, three-quarters of a million people are thought to be living with Obsessive-Compulsive Disorder (OCD) but despite the figures and recent strides in mental health awareness, it’s still misunderstood by those who haven’t experienced it firsthand.
Although many of us might question if we’ve locked the car or turned the hob off, these thoughts are manageable, not obsessional, and don’t impact our day-to-day lives, jobs or social interactions. Living with OCD goes far beyond perfectionism, cleanliness and next-level organisation skills, and to suggest ‘being a bit OCD’ is a personality quirk is undermining the severity of the disorder. A clean home, perfectly styled rainbow bookcase or carefully curated Kardashian cookie jar is an interior styling choice, if anything, not a mental health disorder.
Even if they know their obsessions are not realistic, people with OCD have difficulty disengaging from their obsessive thoughts and compulsions, making it a particularly isolating experience often accompanied with an element of shame and secrecy. The anxiety caused by OCD makes it difficult to resist the urge to carry out a compulsion once an obsession is triggered.
What is OCD?
OCD is a serious anxiety-related condition that affects 1-2% of the UK population (OCD Action), with around half of those cases falling into the severe category. It is typically characterised by two components – recurring intrusive thoughts referred to as obsessions, and compulsive behaviours arising as a result of the anxiety caused by the intrusive thoughts.
Despite how it’s portrayed in the media and in popular culture, it can present itself in many different forms, not just frequent hand washing and checking light switches. According to OCD UK, there are five main categories but it’s possible for obsessions and compulsions to differ from the below or overlap, depending on the individual and the severity of their disorder.
- Checking
- Contamination / Mental Contamination
- Symmetry and Ordering
- Ruminations / Intrusive Thoughts
- Hoarding
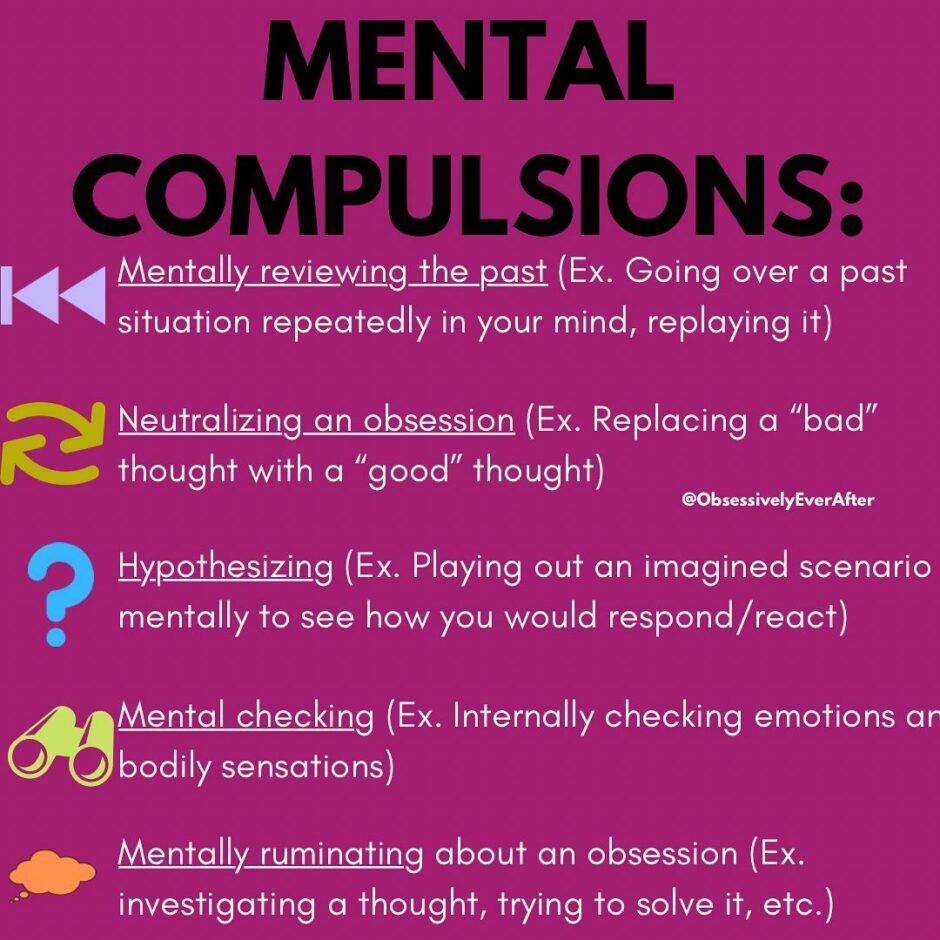
OCD is often referred to as the secret problem, so it isn’t always easy to spot due to the misconceptions surrounding the disorder and the very nature of it being a mental health condition. Some people with Obsessive Compulsive Disorder contend with mental chatter and ruminations, alongside rituals such as repeating words or numbers in their mind until they feel safe to resume, rather than physical compulsions. Pure O (Purely Obsessional), for example, is a type of OCD in which a sufferer has obsessions and mental as opposed to external compulsions, such as trying to stop the thoughts, avoidance or trying to replace unwanted intrusive thoughts with good thoughts.
The average time between the onset of OCD and treatment is 12 years, namely due to the stigma associated with mental health disorders but once diagnosed, OCD can be managed effectively with Cognitive Behaviour Therapy, medication and support groups.
Professor David Veale, one of the Founders of OCD Action and Consultant Psychiatrist in Cognitive Behaviour Therapy explains, “The first treatment for OCD is Cognitive Behaviour Therapy that includes exposure. This means having a good understanding of how your current solutions are maintaining your distress. You then go on to face your fears, to tolerate your anxiety and to test out your expectations. For example, if you have unacceptable thoughts about harming children, it means being with children without any checking that you have not harmed a child or trying to undo a harm that you think you might have done. It also means helping you to reclaim your life.
“As your OCD improves, it’s important to ‘fill the void’ left, deepening your connection with others, and engaging in the work, education and interests that are important to you. Sometimes medication in the form of a SSRI may be helpful in more severe forms of OCD.”
In this interview, we speak to people with OCD to understand what living with the mental health disorder is really like. From how they manage their obsessions and compulsions, seeking professional help and the myths vs reality of having an incredibly misunderstood mental health condition.
Darcey’s Story
How long have you had OCD and what was the road to diagnosis like for you?
I’ve had OCD symptoms since around age 8 I believe, I remember quite clearly as a child constantly having the need to put my tongue to the roof of my mouth and it used to really frustrate me that I couldn’t stop, I now know this was a form of compulsion. I wasn’t actually diagnosed with OCD though until I was 20, I had always been diagnosed with anxiety, although anxiety and OCD quite often go hand-in-hand.
I attended a CBT course for anxiety and said to the woman running it that this course helped but it didn’t pinpoint everything I was feeling, like the need to do a ritual otherwise something bad would happen, even small things like if the volume on the TV was on an odd number I’d be convinced something terrible would happen if I didn’t change the volume to an even number, which meant either I had to change it or I had to vocalise my discomfort to the person controlling the volume. After this, I was quite quickly diagnosed with OCD after discussing more of my compulsions etc, but to be honest even reading up online prior I knew I had it, but I didn’t want to self-diagnose.
Symptoms of Obsessive-Compulsive Disorder (OCD) vary from person to person, what does OCD look like for you and how does it affect your day-to-day life?
My OCD seemed to develop over time and quite slowly, so it began when I was younger having this need to do small compulsions like touching the roof of my mouth and not knowing why I was doing them. Then as I got older I constantly checked things, if I unplugged my straighteners, did I leave the hob on, did I lock the door. I had to check these things multiple times otherwise I’d convince myself something awful would happen and it would be all my fault. This is kind of just like anxiety too, so I think this is why it didn’t get recognised in me sooner.
It was only really in my late teens / early 20’s that I started to feel the full force of OCD. I’d have such distressing thoughts and imagery in my mind of stuff I would never want to do to anyone or myself. This would be towards people I love, my friends, children, animals and even strangers, the thoughts would circle in my mind so much I convinced myself I was a terrible person.
Mentally it is so incredibly draining as it feels like your mind is betraying you, why am I thinking these things? This led to compulsions like doing ‘touchwood’ repetitively in order to feel safe from these thoughts or making a wish at 11:11 every day in order to keep me and my family safe. It really started to affect my daily life as I spent hours thinking about these images, being upset by them and feeling like I couldn’t tell anyone because I was worried about what people would think. OCD also caused me to completely mistrust myself, to the point I’d question my religious views, my sexuality, who I am as a person, how do people view me if I can’t even view myself properly? I know deep down my beliefs and who I am, but OCD makes you question EVERYTHING.
Are there certain triggers for your obsessions/compulsions?
When I’m having a bad spell of OCD anything that is even remotely related to my intrusive thoughts can trigger them, TV, books, daily life. I went through a stage of avoiding things in order to stop the thoughts, but that’s not healthy and really it makes you think about it more. I still, to this day, can’t pick up a kettle without envisioning me spilling the boiling water on me, same with a pan of boiling rice or pasta. I also can’t have volume on an uneven number as it still fills me with fear, but luckily these thoughts don’t affect me as much after a lot of therapy.
Are there certain times or situations when your symptoms worsen?
My symptoms are usually worse when I am having a bad anxious period, this is when the fear behind the intrusive thoughts creeps back in and therefore I find I start to slip back into doing compulsions.
How do you manage living with OCD? Have you explored psychological treatment, support groups or anxiety management techniques?
My OCD has improved greatly due to two main things;
1) I went through a really traumatic period when my Mum was diagnosed with terminal cancer, after this happened I realised that any compulsion I gave into didn’t stop bad things happening to me, especially like making a wish at 11:11. Awful circumstances but since that day we found out I’ve never made a wish at 11:11 or touched wood in order to calm myself and these compulsions took over my life prior.
2) I went to therapy and have been for over a year now, it took quite a while to open up about my intrusive thoughts due to fear of being judged but once I had spoken about them, they instantly began to lose their power. Anyone struggling with OCD, please don’t underestimate how freeing it will be once you speak to a professional.
Whilst there are some external, physical signs & symptoms of OCD, it can also be an invisible mental illness. Can you talk to us about the emotional struggle of living with OCD and how some compulsions are not always quite so obvious?
I think most of my compulsions were within my mind (except for touching wood / my head if there was no wood around ha). I know a few people with OCD who find the ruminating about things the hardest, the thoughts and then the more thoughts about how terrible you must be if you are having those thoughts, they circle around your head for hours. I think that’s the real reality for OCD for most people.
Many people use the phrase “I’m a bit OCD” to describe themselves but there’s an acute difference between, say, liking an organised desk and having OCD. What common misconceptions or assumptions do you find particularly frustrating?
This is the misconception I find the most frustrating! It’s perpetuated by celebrities like Khloe Kardashian who is super organised and tidy, so says she’s super OCD. Of course, I don’t know her medical history, but OCD is so debilitating and exhausting, so when someone makes light of it, you usually know they probably aren’t really experiencing it. The media is to blame as well, with cleaning programmes having people with OCD tidying messy houses. Don’t get me wrong, cleaning and contamination is a real side of OCD, but it’s the tip of the iceberg.
The lack of understanding, even amongst professionals, can be particularly isolating. What changes would you like to see to ensure those living with OCD are seen, understood and supported?
I’d really like large platforms speaking more openly about the less ‘glamorous’ side of OCD. I think seeing others speak about their own experiences is so helpful for others suffering. I found so much peace when I found Instagram and Tik Tok accounts from other people with OCD and realised we all had the same thoughts, I cried for hours after seeing a random video on Tik Tok pop up from someone talking about their experience as I just felt so reassured and heard by it. If it was more openly spoken about, more people would get the help they need from professionals, but because the nature of our thoughts can be so scary and horrendous, people keep it a secret, I certainly did for a while.
Lauren’s Story
How long have you had OCD and what was the road to diagnosis like for you?
I was officially diagnosed with OCD at age 15, but I was struggling with symptoms of OCD many years before I even knew what it was. I was “functioning” with my OCD for more than two years before I hit a “crisis point” when I needed medical intervention, as I was no longer able to function in my everyday life. Once I had my diagnosis, I was put on medication and partook in CBT (Cognitive Behavioural Therapy). Since then, my condition has been very manageable.
Symptoms of Obsessive-Compulsive Disorder (OCD) vary from person to person, what does OCD look like for you and how does it affect your day-to-day life?
My symptoms include a variety of obsessions, compulsions and associated mental health conditions, including depression, anxiety, and some disordered eating. My obsessive thoughts include an irrational fear of harming others by mistake, and a subsequent fear of contamination, an illogical fear that I am unwanted by my friends and family and a large fear of failure. These obsessions lead to compulsions, such as repeatedly checking appliances, hand washing, asking for reassurance and avoiding people or places that may “trigger” my obsessive thoughts.
Currently, my everyday life is largely unaffected by OCD (though I still have some relapses, especially during the pandemic), but before my diagnosis, I would try and neutralise my obsessive thoughts with compulsive behaviour many times every day.
Are there certain triggers for your obsessions or compulsions? Are there certain times or situations when your symptoms worsen?
Unfortunately, the pandemic is a trigger for my obsessive thoughts about contamination. I think that a lot of people with this specific aspect of OCD have been greatly affected by this very uncertain time in our lives. Being in isolation, without any social interaction, worsens my symptoms as I do much better mentally when I am busy. Furthermore, exams are a big trigger for my obsessive thoughts about failure and thus exam periods would be very difficult for me! Luckily, I’m at the stage in my life where I no longer must do exams.
How do you manage living with OCD? Have you explored psychological treatment, support groups or anxiety management techniques?
I manage my depression, a by-product of my OCD, through medication. I have explored CBT and to a lesser extent, DBT (Dialectical Behavioural Therapy), both of which I have found to be very helpful. I find breathing techniques, and distraction to be useful management techniques for my anxiety. I am very lucky that I have a support network of loved ones that I can talk to if I need any help.
Whilst there are some external, physical signs & symptoms of OCD, it can also be an invisible mental illness. Can you talk to us about the emotional struggle of living with OCD and how some compulsions are not always quite so obvious?
One of the hardest parts of living with OCD, for me, is living with something called “intrusive thoughts”. In my case, these involved horrible thoughts of my family and friends being harmed and thus makes me start worrying that I am not doing enough to protect my family. The burden of having to live with these thoughts without knowing what they were or being able to tell anyone (pre-diagnosis) was extremely mentally taxing. Going to school and socialising with friends became something incredibly stressful, rather than a normal part of life to be enjoyed.
One compulsion I had regarding my intrusive thoughts was to think about the thought a lot as if to “neutralise” it. It was as if the more I thought about it, the less scary the thoughts would be. As this part of my illness is invisible, no one knew that I was struggling on a day-to-day basis.
Many people use the phrase “I’m a bit OCD” to describe themselves but there’s an acute difference between, say, liking an organised desk and having OCD. What common misconceptions or assumptions do you find particularly frustrating?
I try to be understanding when I hear things like this, as I know how easy it is to say silly things accidentally. I think the misconception that OCD is about having an incredibly tidy desk is, thankfully, not as commonplace as it used to be. While it is a little frustrating that some people assume that having OCD is just about turning light switches on and off, the thing that frustrates me most is ignorance in the face of education. If you listen to people’s experiences and learn from what they are saying, you are doing everything right, in my opinion.
The lack of understanding, even amongst professionals, can be particularly isolating. What changes would you like to see to ensure those living with OCD are seen, understood and supported?
While I have been lucky in the sense that I have always had a positive and professional experience when talking to doctors about my condition, I have had negative experiences with mental health professionals in schools. When I was 17, I had a lot of my support system for exams removed, as I seemed on the surface to not need it. This was against the advice from my doctor. I found this to be devastating as I did not feel like the invisible nature of my condition was understood by these professionals. More education and funding for supporting young people with OCD in schools should be a priority. If you are unsure how best to support someone with OCD, don’t be afraid to ask. With the right support and treatment, people with OCD can (and do) live a very full and happy life.
Ellie’s Story
How long have you had OCD and what was the road to diagnosis like for you?
While I was only recently diagnosed (early September), I’ve struggled with OCD symptoms since I was fourteen years old. I found it hard talking about my symptoms – intrusive thoughts & compulsions were rarely spoken about in the media I was consuming! It was only when I turned seventeen that I started to read up on what could be causing these distressing thoughts. I put getting professional help off for a while, shrugging it off as being ‘not important enough’ (reality check: any mental health problem, big or small, is important!) but thankfully, with the support of loved ones, I reached out to medical professionals & a cognitive behavioural therapist – and that was that.
Symptoms of Obsessive-Compulsive Disorder (OCD) vary from person to person, what does OCD look like for you and how does it affect your day-to-day life?
OCD for me is a very subtle & invisible mental illness. It was very easy for me to put on a brave face & perform as if all was ok, when in reality, it wasn’t. Inside my head were intrusive thoughts that genuinely scared & frightened me. Thoughts of loved ones or myself in danger or in harm’s way seemed to lurk around each corner. My main struggle was compulsions. Whenever I’d have an intrusive thought, I’d compulsively have to tap anything five to twenty-five times. It was exhausting – I can’t explain where it came from or why it eased the thoughts, but deep down I knew it wouldn’t prevent anything. If I didn’t do it, I’d panic. It was like my body was forcing me!
Are there certain triggers for your obsessions or compulsions?
I had certain triggers – horror movies being my biggest one. For some reason, in my head, I would replace the characters I was watching on screen experiencing these terrible fates with myself, and people I knew in real life. It was nasty (having a horror-obsessed boyfriend wasn’t helping!) & honestly, made me feel more childish than I was. I had to be SO weary of the media I was consuming. So frustrating! Hearing of any sad event in someone’s life made me automatically think ‘that will happen in my life’ and happy events made me think ‘this is too good to be true – something bad is ought to happen’.
Are there certain times or situations when your symptoms worsen?
Thankfully I could go a while sometimes without experiencing my compulsions. Periods of high stress or emotion made everything so much worse, which is to be expected. As an anxious person in my day to day life, I would often become overwhelmed and have a short burst of constant intrusive thoughts and tapping things over and over.
How do you manage living with OCD? Have you explored psychological treatment, support groups or anxiety management techniques?
Living with OCD now is much easier than it was, now that I’m aware of it. It’s not this monster without a face anymore, it’s something I can name and talk about. My therapist taught me to recognise that I am not my thoughts, no matter how awful they are. These intrusive thoughts do not make me a horrible person for thinking them, nor do they represent what I truly want in life. Finding the evidence for my thoughts (usually there would be none!) and evaluating the true likelihood of them becoming reality was hard to master, and much easier said than done – yet once I did, it truly changed my life.
Whilst there are some external, physical signs & symptoms of OCD, it can also be an invisible mental illness. Can you talk to us about the emotional struggle of living with OCD and how some compulsions are not always quite so obvious?
Having OCD was an emotional rollercoaster. The frustration & guilt was the awful part. When you experience thoughts of bad things happening to those you truly love, it changes the way you view yourself as a person. While the thoughts didn’t define me as a person, I thought I was evil and inhumane. How dare I think these things? Why am I thinking these things? Am I a bad person? It was like having the little devil on your shoulder – yet they aren’t whispering as they do stereotypically, they’re shouting & screaming.
Many people use the phrase “I’m a bit OCD” to describe themselves but there’s an acute difference between, say, liking an organised desk and having OCD. What common misconceptions or assumptions do you find particularly frustrating?
“I’m a bit OCD.” We’ve all said it. Whether you like things in colour order, hate mess or must have your shoes in a particular order, this phrase is more common than it ever should have been. It takes the importance away from this mental illness and instead turns it into this adjective to be used for enjoying things that most of us like – organisation & cleanliness. It almost belittles the issue and brushes it under the carpet. Never to be spoken about.
The lack of understanding, even amongst professionals, can be particularly isolating. What changes would you like to see to ensure those living with OCD are seen, understood and supported?
I wish more people would try to understand. It’s hard, I appreciate that. But little steps change the most! If people could be more open-minded about OCD, that would do a whole world of good. People I’ve spoken to about intrusive thoughts have genuinely said things like “gosh, that’s a bit freaky of you”. While it’s a lot to take in and understand, us intrusive thoughts & compulsions – having humans can’t control them! We’re not freaks & our thoughts and compulsions don’t make us strange or any different from you.
We need support and we need compassion from others. I’ve found that OCD is one of the least spoken about mental illnesses, especially in secondary schools. If it ever is mentioned or represented in the media, it’s almost always the same type. More diverse representation and more education to provide a better understanding of OCD would be an absolutely amazing thing for everyone.
Olivia’s Story
How long have you had OCD and what was the road to diagnosis like for you?
I have had OCD for about 8 years now. I started experiencing symptoms in January 2014 and did not get diagnosed until 10 months later. I was only 16. The road to diagnosis was a hard one, I think this was primarily because of my family’s lack of knowledge around mental illness and our finances at the time. When it first started I didn’t really understand what was happening to me, I thought I was going crazy. At the time I didn’t feel comfortable talking to anyone about it so I ended up self-diagnosing from researching how I felt online. My parents eventually brought it up with me and we decided I should see someone about it, by that time it had gotten so severe I couldn’t hide it anymore. Mental health care professionals can be really expensive so it took time for my parents to find the money for me to see one. Eventually, I saw a psychologist and she diagnosed me with OCD, General Anxiety, Sleep Apnea and insomnia.
Symptoms of Obsessive-Compulsive Disorder (OCD) vary from person to person, what does OCD look like for you and how does it affect your day-to-day life?
My symptoms really change depending on the context and how I am feeling internally. Because I have had OCD for 8 years now I am pretty good at knowing what places and situations trigger me, but it can be hard to communicate those needs to other people. If I am having a particularly hard day with it I will just stay home and avoid people because it is most controllable in a familiar space. I know that when I am stressed or tired I will feel it the worse so I always have to prepare myself mentally for days like that. I do have some friends who are great with me about it but whenever I do have to explain it to someone it gets worse because I feel totally insane describing what I feel!
Are there certain triggers for your obsessions or compulsions?
My biggest trigger is with anything that lathers or foams, so washing my hands, showering, brushing my teeth and household cleaning takes a lot longer than what’s typically normal. I will always opt for sanitiser over washing my hands and will only wash my hair when I have to. Walking on surfaces that have lines or cracks can be difficult too, I always try not to look at my feet when I am walking in case I get trigged. I also tend to develop obsessions about the placement of my hands when I’m sitting or how my feet are placed when I’m standing. Honestly though, when my OCD is at its worse anything and everything will trigger me, I just have to look at something and I’ll develop an obsession!
Are there certain times or situations when your symptoms worsen?
I am currently doing my master’s degree and I know that when an assessment or exams are coming up I’m going to feel it. Avoiding stress and emotional distress are key for me to contain my OCD. In 2020 I lost three of my grandparents in one year and when I was dealing with that grief my OCD got worse. But totally avoiding negative stress and emotions is impossible so for me it’s all about preparing myself mentally and self-compassion!
How do you manage living with OCD? Have you explored psychological treatment, support groups or anxiety management techniques?
I think for a long time I didn’t manage it, I just went every day being pushed to my mental limit. I didn’t find that the first psychologist I saw helped me so I was pretty sceptical about trying another therapist. However, in 2020 I found a Counsellor who really helped me deal with the trauma which caused me to develop OCD and in the process, I have been able to get a handle on my OCD rather than it having a hold on me! Exposure therapy has also been key for me, fighting my compulsions has helped reduce the severity of them over time. I also use a CBT app which helps me feel in touch with my emotions and body.
Whilst there are some external, physical signs & symptoms of OCD, it can also be an invisible mental illness. Can you talk to us about the emotional struggle of living with OCD and how some compulsions are not always quite so obvious?
Living with OCD can definitely be really hard, especially if you are doing it alone. Before I got treatment for it there were days where I didn’t think I could do it anymore. It’s like constantly having a voice in your head telling you to do something that is totally crazy and unnecessary but is the only thing that will make you feel better. Dealing with my past trauma was definitely key to overcoming the emotional battle I was having because of my OCD, it allowed me to develop self-compassion for why I had OCD in the first place and a sense of gratitude toward myself for finding a way to cope in a time that was really terrible!
Many people use the phrase “I’m a bit OCD” to describe themselves but there’s an acute difference between, say, liking an organised desk and having OCD. What common misconceptions or assumptions do you find particularly frustrating?
Yes! I think that phrase is the easiest way for someone to make a person with OCD feel small and even more crazy than they already do! comments like that can really hurt someone battling it; especially if they don’t have the voice to correct them. But the biggest misconception I find frustrating is when people limit what OCD can look like, OCD isn’t just about washing your hands or organising how some books look! OCD can look a myriad of ways and ultimately looks like whatever it does to the person who has it!
The lack of understanding, even amongst professionals, can be particularly isolating. What changes would you like to see to ensure those living with OCD are seen, understood and supported?
I would love to see more therapists specialise in helping people with OCD, especially becoming aware of the different types of OCD and the non-medical options people have to overcome it. A lot of people who have OCD are prescribed medication and are never told what other treatment options there are! It would also be great to see some tools developed to help people explain what OCD is like to friends and family easier!
Caitlin’s Story
How long have you had OCD and what was the road to diagnosis like for you?
I’ve had OCD for (I think) about 7 years now, as I started to experience it while I was at college. It started with checking and hand-washing compulsions, and it was actually something my mum pointed out to a doctor when I was at an appointment for something else. I was then referred to a mental health specialist, who talked to me about what I was experiencing and gave me information on OCD.
This wasn’t something I’d even thought I could have, despite looking up information on things like OCD and anxiety online, so it was quite the shock! I also had to fill in both the general mental health questionnaire and also one called the OCI (Obsessive Compulsive Inventory) which gave the specialist more of an idea about which type(s) of OCD I had. I’ve not tried medication for it, but I’ve done Exposure and Response Prevention, which is the gold standard treatment, and this worked well for me! I’m actually not sure how the diagnosis and support system works, but I’ve been treated for OCD on several different occasions both privately and on the NHS, and also declared it to my uni while I was there. I’ve never applied for disabled students allowance or anything like that though, so I can’t offer any insight on that, although I know that students with OCD were encouraged to at my uni.
Symptoms of Obsessive-Compulsive Disorder (OCD) vary from person to person, what does OCD look like for you and how does it affect your day-to-day life?
My OCD was noticed because it manifested in quite a physical way – I washed my hands so much that it made them really dry and cracked, especially on the back, around my wrist. At my worst, during my first year of uni, I was spending a shocking amount of time washing my hands – I would soap up and rinse them over 30 times, and this meant my new friends would often have to wait for me so we could go to eat dinner together. I would go through a bottle of liquid hand soap a week, and also used a lot of hand sanitiser while I was out and about. I would also have to use lots of hand creams to try and stop my hands from being damaged. I’m doing a lot better now, even with COVID, but I still wash my hands a lot. I often worry that people will judge me at work for it, and I’ve only ever admitted to having ‘a bit of a thing about germs’ because I’m worried it’ll affect my job if people know.
It also manifested as a lot of checking – sometimes this would involve checking ‘sensible’ things like doors being locked, or the stove being off, but I was also incredibly afraid of having posted something unpleasant on social media/email without knowing about it so I would get caught in a vicious cycle of checking and refreshing everything (usually at night, so it started to affect my sleep). It got to a point where I avoided almost all social media for several years, but I’ve slowly introduced almost everything back into my life. I still sometimes check things, both the ‘sensible’ and the social media, and can still find myself compulsively screenshotting things I’ve posted ‘just in case’.
Are there certain triggers for your obsessions or compulsions?
I’m most often triggered by things not feeling/being ‘clean’ – if I’ve touched something I would have to wash my hands before touching my face, or eating/preparing food. This is somewhat ironic to me, considering my job at the moment involves a lot of mud! If I see a fly land on my food or glass, that’s quite upsetting to me. COVID has also been quite a big trigger, but I was always careful about washing my hands (etc) anyway, and I try to follow the rules about social distancing and masks as best I can.
I can also be triggered by social media – by feelings of something not being ‘right’, or when I want to go to sleep I might still feel the need to check. For this reason, there are certain social media sites I avoid. I’m also really frightened by the idea of computer viruses or accounts being hacked, so I can be really wary of things my friends send me like YouTube/TikTok links etc.
On one very memorable occasion, OCD was used in the crime show Criminal Minds (which I used to be a big fan of), and this upset my OCD as it caused me to worry that I, like the character with the disorder, would commit some horrible crime. This is because OCD is something that goes against your values – it wants to convince you that you’re a horrible person and are putting people in danger. I often worry about things happening to my friends or family for this reason, and OCD convinces me I’m responsible for ‘preventing’ the bad things.
Are there certain times or situations when your symptoms worsen?
It seems that my OCD has been at its worst when I’ve gone through a big life change – like starting uni, for example. This is something that goes into the plan you make at the end of a limited course of therapy sessions – you talk about and note down anything that might trigger the OCD and/or cause it to worsen. I would definitely count the pandemic as one of these times – there was a point where I could barely get dressed during lockdown due to the thought of germs being on my clothes and my hands/feet, and the constant messages on TV/social media about washing hands wasn’t helpful either! I think that a breakup might also be one of those times, especially if I’ve been hiding my OCD from the person, but with that, it’s more about coping with feelings of being ‘unlovable’ or ‘a freak’ – it’s easy to blame mental health for these things, even if it’s just a case of being incompatible. On a smaller scale, my symptoms can be worse before important events or dates – I used to worry about getting sick before or on the day of trips/exams (etc) and I also find I worry about becoming ill at work, so I get warier of certain foods (e.g. not eating a lot of dairy as large amounts can make me ill) and food safety.
How do you manage living with OCD? Have you explored psychological treatment, support groups or anxiety management techniques?
I’ve tried a lot of things over the years, from meditation and yoga (fun and relaxing, but not specifically helpful for my OCD) to Cognitive Behavioural Therapy and Exposure and Response Prevention. CBT and ERP are considered ‘gold-standard’ treatments, and I’ve been able to manage my OCD really well (with the help of a therapist) using them, but it’s a lot of homework – there’s no easy fix, but it’s worth it. I had tried a support group in the past, which helped me to feel less alone, and there was a student-run support group at my uni that was absolutely invaluable during that first year, but I found one-on-one treatment more effective when I could access it. In terms of everyday stuff, I’ve tried to push myself outside of my comfort zone by getting a job, but I’ve also found video games, books, writing and general fandom culture to be a really helpful distraction and form of stress relief.
Getting my job was something I tried to just do, rather than overthinking it and avoiding it like the OCD would want – it was a lot to adjust to, but I was fortunate enough to be in a place where I could handle it and it provided great opportunities and distractions. It’s also really nice to have friends and family that try their best to understand my OCD without enabling it or ‘feeding’ it, but on balance, there are lots of people that don’t know, especially at work, and that can be hard.
Whilst there are some external, physical signs & symptoms of OCD, it can also be an invisible mental illness. Can you talk to us about the emotional struggle of living with OCD and how some compulsions are not always quite so obvious?
I’m fortunate that my OCD began in a way that was externally visible and pretty stereotypical, but it’s not always been like that. One of the main emotional things I’ve struggled with over the years is that feeling of being a ‘freak’ or a ‘bad person’ – it can be hard to explain obsessions and compulsions, and sometimes the thoughts can be so horrifying that you worry about admitting them in case you’re treated like a criminal or a ‘crazy person’. Of course, these are thoughts and images specifically created by the OCD to get a reaction from you (like a bully) – they’re ‘egodystonic’ which means they go against your values, and attack the things that are important to you such as your friends, family, health and reputation. It would have taken me a lot longer to find help if my OCD only consisted of those thoughts and images, as this isn’t something many people associate with the disorder due to the ‘clean and organised’ stereotype. People with OCD might worry that they’ll cause physical or emotional harm, or that they’re a bad person, due to thoughts that go against their morals/religions – I worry sometimes that I’ve said something awful to a friend or stranger, even though it’s something I would never do.
Some days it’s difficult to accept that I have OCD and that it’s something that’ll be a part of me forever – however, I know that with a bit of work I can (and do) manage it, so it’s not all doom and gloom! It also feels rarer than, say, depression or anxiety, so sometimes it feels a bit harder to find people I can relate to. That being said, one of my best friends was recently diagnosed with OCD, so it’s good to know that we’ll be able to support each other through it.
Many people use the phrase “I’m a bit OCD” to describe themselves but there’s an acute difference between, say, liking an organised desk and having OCD. What common misconceptions or assumptions do you find particularly frustrating?
The “I’m/you’re a bit OCD” thing really annoys me, as it trivialises the condition and stops people that are being seriously harmed by the disorder from seeking help. I’ve seen it thrown around as an insult on pages meant to be for cleaning tips, and at my first job back in college I was told “don’t be OCD about this task”…that was fun to hear as someone coming to terms with actually having OCD! Hearing it constantly referred to in an insulting or negative light can really add to the feelings of isolation and self-loathing, those feelings of being ‘a freak’.
The ‘clean and organised’ stereotype can also do a lot of harm, as it means people suffering with other types of OCD such as harm OCD or Pure O don’t even associate their symptoms with the disorder. Sometimes it’s a little awkward for me to admit to the germaphobic aspect of my OCD as it can fuel the stereotype, but I can tell you now that my room is not nearly as clean or organised as you might expect! Indeed, even with the most stereotypical form of OCD, I didn’t realise I had it, so anything that perpetuates misconceptions can be really harmful.
The lack of understanding, even amongst professionals, can be particularly isolating. What changes would you like to see to ensure those living with OCD are seen, understood and supported?
I think having more awareness of how OCD can be for real people is important (I’m really happy to see Zoella looking into this, and happy to help out!). There are a lot of social media accounts run by trained therapists and people with OCD that are really informative as well which helps (though of course, you have to be careful about misinformation). Charities like Mind and OCD Action are really useful too, as they can provide information and support for the sufferer and also friends/family, and it’s quite easy to access and understand. Depictions of OCD in TV/film that are realistic and not treated as a joke can also be helpful, and can give people characters to look up to (similarly, celebs being honest about their experiences of the disorder can be positive too). It’s a big ask, but I’d love to see the end of “I’m/you’re a bit OCD” – it’s not helpful and it really gets on my nerves, even if the person means well!
I also think that an awareness of OCD would be helpful at the college/university level, and in the NHS – my main barrier to help was that I got kind of… funnelled through the university and NHS systems in a way that pointed me to the wrong kind of treatment initially (one that was more general, made to deal with general uni stresses and anxieties), when I should have been on a more specific form of treatment that actually worked really well when I got to it! One of the most helpful things during that difficult first year was simply feeling seen and cared for by the student welfare team at my uni – they made sure I made and went to appointments, and helped me to feel less alone. Indeed, I was able to poke fun at a shared OCD experience with one of them, a fellow sufferer, because we could connect and understand how truly strange OCD can be.
Violet’s Story
How long have you had OCD and what was the road to diagnosis like for you?
I’ve officially had OCD for nearly 4 years, however, I personally think I have had it for around 5/6. The road to diagnosis for me was difficult, I went through CAMHS which did take a while (as most people know) but 2020 was the year I finally got to the top of the list and started to receive therapy.
Symptoms of Obsessive-Compulsive Disorder (OCD) vary from person to person, what does OCD look like for you and how does it affect your day-to-day life?
For me, my OCD was mainly Reassurance, Germ and Ritual OCD. This means I was washing my hands habitually almost every hour. After using the toilet I’d spent at least 5 minutes at the sink making SURE they are clean. From this, my OCD stemmed to ritual OCD in which where I would have to do something a certain amount of times, this was things from light switches to locking the doors. This is where the Reassurance OCD came in and I would stay up after everyone else and spend at least 20 minutes a night making sure all doors are locked and switches are off, this was all reassuring me that my family would be safe which was a big part of my OCD.
A lot of my OCD was family-based. My main trigger would be dripping taps, this is because I didn’t want to waste any money, and later figured that I’d been told as a child that “every drip is worth a penny, so make sure the tap is OFF”, which every child gets told, to make sure they turn off the tap as it wastes water! However in my head, the OCD took this information and twisted it, so I would make sure the tap is definitely off because I didn’t want my mum (who is a single parent and works so hard for her children) to waste money on a drippy tap. Additionally, I also had intrusive thoughts, this came in the forms of “if I don’t do this then something bad will happen”.
Are there certain triggers for your obsessions or compulsions?
I suffer from depression as well, so a low mood is a huge trigger. Right now there are very few triggers for me. One big one was obviously COVID, having had OCD before COVID, when the virus came around my OCD was probably at its peak and the fact a deadly virus was going around didn’t help! My main trigger was the dripping tap. Any time I would see a tap drip, I’d have to keep checking it’s off, keep touching it so it stays off.
Are there certain times or situations when your symptoms worsen?
When around lots of people, being in places I don’t know are clean. Fatigue and tiredness.
How do you manage living with OCD? Have you explored psychological treatment, support groups or anxiety management techniques?
I’ve received CBT via CAMHS. The therapy lasted around 6 months. Through the therapy I was taught so many techniques, one of the ones I still use is ERP. ERP is Exposure Response Prevention. Although it may seem weird, one of my targets was to simply sit in front of the sink and watch the tap drip. By doing this once and seeing after that in fact nothing bad did happen, I began to see things a lot differently!
Whilst there are some external, physical signs & symptoms of OCD, it can also be an invisible mental illness. Can you talk to us about the emotional struggle of living with OCD and how some compulsions are not always quite so obvious?
For me personally, my OCD had a huge impact on my emotions and general mental health. I’d hear a lot of the time people saying at school and college “oh I’m so OCD” and “omg you’re triggering my OCD” and I’d think to myself how little they actually know, I’d think how they have no idea that I was counting how many people touched the door handle, and how I would be about to ask to go to the toilet just to wash my hands again but most of all, how I was about to go home and the compulsions would start all over again and it would mean another restless night. It became difficult as well to tell some of my friends, I’d tell them that I have been diagnosed with OCD and I distinctly remember one moment, where I felt so insignificant and silly for telling them, a friend said “oh well yeah everyone’s a bit OCD”. I remember after she said that I smiled and agreed and went home later and cried a lot.
Many people use the phrase “I’m a bit OCD” to describe themselves but there’s an acute difference between, say, liking an organised desk and having OCD. What common misconceptions or assumptions do you find particularly frustrating?
This leads on nicely from what I was just saying! For me a huge misconception is people thinking and assuming that OCD is just being super clean and organised. It really is not. Of course for some, part of their OCD is being really organised (me included) but anyone can be organised. A good way I like to explain it is that, anyone can organise their pens in colour order, but those with OCD may do this over and over and over until they feel satisfied.
The lack of understanding, even amongst professionals, can be particularly isolating. What changes would you like to see to ensure those living with OCD are seen, understood and supported?
For me, I’d like to see a bigger focus on the understanding of the indirect impact that OCD can have on an individual and their loved ones. For example, my OCD at one point meant that my mum struggled to sleep most nights as she was awake making sure I wasn’t washing my hands for too long, or wasn’t checking the doors too much.
Personally, I think OCD is one of the few disorders that people do not know enough about. I personally believe there is definitely a lack of professionals who know what and how to help OCD. Additionally, something I really think is necessary is for mental health to be taught in schools, for children and young people to learn what different mental health conditions mean and how they can identify and help them.
If you’re struggling with OCD, you can get help here at ocduk.org or ocdaction.org.uk